Oral Surgery at HRTD Dental Services, Mirpur-10
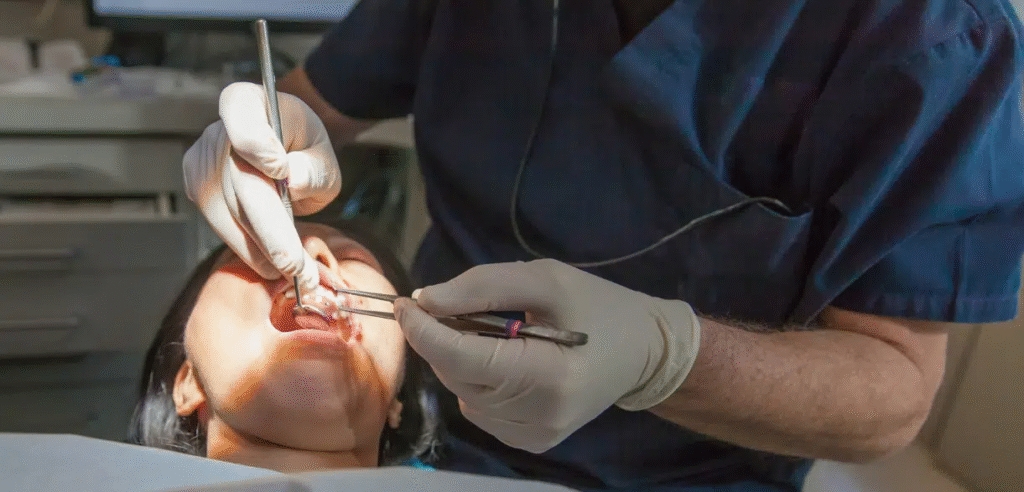
HRTD Dental Services in Mirpur-10, Dhaka provides expert oral surgery for patients seeking advanced dental care. The clinic specializes in a wide range of procedures, including tooth extractions, wisdom tooth removal, dental implant placement, jaw correction (orthognathic surgery), cyst and tumor removal, and frenectomy. Each procedure is performed by experienced oral and maxillofacial surgeons, ensuring safety, precision, and optimal outcomes.

Address: House # 10/1, Road # 10, Mirpur-10, Dhaka, Bangladesh
Phone: +880 1797-522136 | +880 1987-073965 | +880 1784-572173
The clinic follows a patient-centered approach, beginning with a comprehensive consultation that includes dental examination, imaging, and treatment planning. This allows the surgeons to tailor the procedure according to the patient’s specific needs. HRTD Dental Services emphasizes minimally invasive techniques wherever possible, reducing discomfort and speeding up recovery.
Post-operative care is an integral part of their service. Patients receive detailed instructions on pain management, oral hygiene, diet, and follow-up appointments, ensuring smooth healing and long-term oral health.
HRTD Dental Services also maintains affordable pricing for oral surgery in Bangladesh without compromising quality. Modern equipment, a sterile environment, and friendly staff make it a trusted choice for families and individuals in Dhaka.
Professional care, advanced techniques, and patient comfort make HRTD Dental Services a top destination for oral surgery in Dhaka.
What Is Oral Surgery?
Oral Surgery is a specialized branch of dentistry focused on the surgical treatment of conditions involving the mouth, teeth, gums, and jawbone. It is performed when conventional dental procedures like fillings, scaling, or root canal treatments are not sufficient to solve a particular problem. Oral surgery helps manage complex cases such as impacted wisdom teeth, jaw misalignment, facial trauma, or dental implant placement. The treatment is usually performed by an Oral and Maxillofacial Surgeon, a dental specialist with advanced training in surgical techniques.

Oral surgery plays an important role in restoring oral health, functionality, and aesthetics. Through surgical intervention, patients can regain their ability to chew properly, speak clearly, and maintain a natural facial appearance. It is not limited to teeth alone—it also includes procedures involving the jaw joints, soft tissues, and bone structures of the mouth and face.
There are various reasons a patient might need oral surgery. Some teeth, especially wisdom teeth, may grow in an improper position or remain trapped under the gum, causing pain or infection. In such cases, surgical extraction is required. Similarly, individuals who lose one or more teeth often need dental implant surgery to replace the missing teeth permanently. Oral surgery is also required to remove cysts or tumors that develop inside the mouth, repair jawbone deformities, or treat facial injuries caused by accidents.
Unlike regular dental treatments, oral surgery involves deeper tissues and structures of the oral cavity. For instance, while a dentist can remove surface-level tooth decay or perform a root canal to clean an infected tooth, an oral surgeon deals with more advanced cases that affect the bone or require reconstructive procedures. Oral surgery is often performed under local or general anesthesia to ensure patient comfort and precision during the operation.
The benefits of oral surgery are both functional and aesthetic. It relieves pain, removes infections, restores the natural alignment of teeth and jaws, and enhances overall facial balance. In many cases, it also prevents more serious oral health problems in the future by addressing the root cause of the issue rather than only treating symptoms.
Oral surgery is performed by an Oral and Maxillofacial Surgeon, who has undergone years of additional education and hands-on training after completing dental school. These specialists are skilled in handling complex surgical procedures involving bones, nerves, and soft tissues of the oral and facial regions. They work closely with general dentists and other specialists to ensure comprehensive and safe treatment for each patient.Oral Surgery
In essence, oral surgery is an advanced dental discipline that focuses on the surgical correction and treatment of complex oral, dental, and facial conditions, helping patients regain comfort, confidence, and long-term oral health.
Why Is Oral Surgery Needed?
Oral surgery is often necessary when conventional dental treatments cannot adequately address certain problems in the teeth, gums, jaw, or surrounding facial structures. While routine dental procedures such as fillings, cleanings, or root canal treatments handle minor or moderate dental issues, some conditions require surgical intervention to restore oral health, function, and aesthetics.
One of the most common reasons for oral surgery is impacted or problematic wisdom teeth. Wisdom teeth, or third molars, often do not have enough space to emerge properly, leading to pain, swelling, infection, or even damage to neighboring teeth. In such cases, oral surgery is performed to safely remove the impacted teeth and prevent further complications.
Another reason for oral surgery is tooth loss. Missing teeth not only affect appearance but also impact chewing and speaking. Dental implants, which involve surgically placing a titanium post into the jawbone, are a common oral surgery procedure to replace lost teeth. This approach provides a permanent and natural-looking solution that maintains jawbone structure and prevents bone deterioration.Oral Surgery
Jaw-related problems are also a significant reason for oral surgery. Conditions like misaligned jaws, underbite, overbite, or temporomandibular joint (TMJ) disorders may require surgical correction to restore proper function and alignment. Jaw surgery, also known as orthognathic surgery, helps patients improve bite function, facial symmetry, and overall oral health.Oral Surgery
Oral surgery is also indicated for removing cysts, tumors, or growths in the mouth. Cysts and tumors can develop in the jaw or soft tissues and, if left untreated, may lead to infections, bone damage, or other serious health issues. Surgical removal is often the most effective way to prevent complications and ensure the patient’s safety.
Trauma or injury to the mouth and face is another common reason for oral surgery. Accidents that cause broken teeth, fractured jawbones, or soft tissue injuries often require surgical intervention to repair the damage, restore function, and prevent long-term complications.
In some cases, frenectomy or surgical procedures to correct tongue or lip tie are necessary to improve speech, eating, or oral hygiene. Oral surgery can also be performed for aesthetic improvements, such as correcting irregularities in the jaw or gum tissue to enhance a patient’s smile.
Ultimately, oral surgery is needed whenever a dental or oral condition cannot be effectively treated through non-surgical methods. The procedure addresses the root cause of the problem rather than just alleviating symptoms, providing long-term benefits for oral health, functionality, and facial appearance.
By consulting an Oral and Maxillofacial Surgeon, patients receive expert care tailored to their specific condition. The surgeon evaluates the complexity of the problem, discusses the available treatment options, and performs surgery with precision and safety. This ensures that the patient can achieve optimal results, recover comfortably, and maintain long-term oral health.
In conclusion, oral surgery is essential for impacted teeth, tooth replacement, jaw misalignment, cysts or tumors, trauma repair, and functional or aesthetic improvements. Without it, many oral health issues could progress, causing pain, infection, or permanent structural problems.
Types of Oral Surgery
Oral surgery encompasses a wide range of surgical procedures designed to treat complex dental and facial conditions. These procedures address issues that cannot be resolved with routine dental care, such as fillings or cleanings. Oral surgery can improve oral health, restore function, relieve pain, and enhance facial aesthetics. Below is an overview of the most common types of oral surgery.
1. Tooth Extraction
Tooth extraction is one of the most common oral surgeries. It involves the removal of a damaged, decayed, or problematic tooth that cannot be saved through restorative treatments. Extractions are necessary for teeth affected by severe decay, infection, or trauma. Impacted teeth, especially wisdom teeth, often require surgical extraction when they fail to emerge properly.
2. Wisdom Tooth Surgery
Wisdom teeth, or third molars, can often cause complications if there is insufficient space in the jaw. They may become impacted, partially erupted, or grow at an abnormal angle. Oral surgeons remove these teeth surgically to prevent pain, infection, crowding, or damage to adjacent teeth. This procedure is usually performed under local or general anesthesia, depending on the complexity.
3. Dental Implant Surgery
Dental implants are a modern solution for replacing missing teeth. This procedure involves surgically placing a titanium post into the jawbone, which acts as an artificial tooth root. After proper healing, a crown is attached to the implant, providing a durable, natural-looking replacement. Implants require surgery because the post must integrate with the jawbone for stability.
4. Cyst and Tumor Removal
Cysts and tumors can develop in the jawbone or soft tissues of the mouth. Some are benign, while others may pose a risk of serious complications. Oral surgery allows for precise removal of these growths, preventing further damage to surrounding teeth, bone, or tissues. A biopsy is often performed during surgery to determine whether the growth is benign or malignant.
5. Jaw Surgery (Orthognathic Surgery)
Jaw surgery, also called orthognathic surgery, corrects abnormalities of the jaw and facial structure. This includes issues like overbite, underbite, or jaw misalignment. Surgery can improve bite function, speech, and overall facial symmetry. In many cases, jaw surgery is combined with orthodontic treatment to achieve the best results.
6. Frenectomy
A frenectomy is a surgical procedure to release a tight or restrictive frenulum in the mouth, commonly referred to as a tongue tie or lip tie. This procedure can improve speech, eating, and oral hygiene, especially in infants and children.
7. Trauma Surgery
Trauma to the face, teeth, or jaw can occur due to accidents, sports injuries, or falls. Oral surgeons repair fractures, reposition displaced teeth, and restore soft tissues. Surgical intervention ensures proper healing, prevents long-term complications, and restores facial function and appearance.
8. Bone Grafting
Bone grafting is often performed before dental implants or to repair jaw defects. It involves adding bone tissue to the jaw to provide a stable foundation for implants or to reconstruct areas affected by trauma, disease, or bone loss.
9. Oral Biopsy
An oral biopsy is a surgical procedure in which a small tissue sample is removed from the mouth for diagnostic purposes. This helps detect oral cancers, infections, or other abnormalities. Early detection through biopsy can save lives and prevent severe complications.
10. Soft Tissue Surgery
Soft tissue surgeries involve the gums, lips, or other oral mucosa. Procedures may include removing excess gum tissue, reshaping gums for aesthetic purposes, or correcting lesions and growths.
Overall, oral surgery covers a wide range of procedures that restore function, prevent complications, and improve oral and facial aesthetics. Each type of surgery is tailored to the patient’s specific condition, and careful planning ensures safe and effective outcomes.
Wisdom Tooth Extraction Surgery
Wisdom tooth extraction surgery is one of the most common oral surgical procedures performed worldwide. Wisdom teeth, or third molars, usually appear between the ages of 17 and 25. While some people have enough space in their jaws for these teeth to erupt normally, many experience complications due to insufficient space or improper alignment. These issues often require surgical removal to maintain oral health and prevent further dental problems.
Why Wisdom Tooth Extraction Is Needed
Wisdom teeth can cause several problems if they do not erupt properly:
- Impaction: The tooth remains trapped under the gum or jawbone.
- Partial eruption: Only part of the tooth breaks through the gum, making cleaning difficult.
- Crowding: Wisdom teeth can push adjacent teeth, causing misalignment.
- Infection or gum disease: Partially erupted teeth create spaces where bacteria can accumulate, leading to pain, swelling, or infection.
- Cysts or tumors: In rare cases, impacted wisdom teeth may contribute to cyst formation, which can damage the jawbone and surrounding teeth.
The Procedure
Before surgery, the oral surgeon evaluates the position and condition of the wisdom teeth using X-rays or 3D scans to plan the safest approach.
- Anesthesia: Depending on the complexity, local anesthesia, sedation, or general anesthesia is used to ensure the patient is comfortable and pain-free.
- Incision and Exposure: If the tooth is impacted, an incision is made in the gum to expose it. Sometimes, a small portion of the jawbone covering the tooth may also need to be removed.
- Tooth Removal: The tooth may be removed in sections, especially if it is fully impacted or angled abnormally.
- Cleaning and Closure: After removal, the area is cleaned to remove debris. The incision may be stitched closed with dissolvable sutures.
Recovery and Aftercare
Recovery usually takes a few days to a week, depending on the complexity of the surgery. Important aftercare steps include:
- Applying an ice pack to reduce swelling.
- Avoiding hard, chewy, or hot foods for the first few days.
- Taking prescribed painkillers and antibiotics to prevent infection.
- Maintaining oral hygiene using gentle rinses to keep the extraction site clean.
- Avoiding smoking or using straws, as suction can dislodge the blood clot and cause a painful condition known as dry socket.
Benefits of Wisdom Tooth Extraction
- Relieves pain and discomfort caused by impacted teeth.
- Prevents infection, gum disease, and decay in surrounding teeth.
- Reduces the risk of misalignment or crowding of adjacent teeth.
- Prevents jaw cysts or other complications associated with impacted wisdom teeth.
Wisdom tooth extraction is a preventive and therapeutic procedure that addresses potential dental problems before they worsen. Timely removal not only relieves pain but also protects the long-term health of the teeth, gums, and jaw.
Surgical Tooth Removal
Surgical tooth removal, also called surgical extraction, is a procedure performed to remove teeth that cannot be extracted using simple methods. Unlike a routine tooth extraction, surgical removal is often required when a tooth is impacted, broken, or positioned abnormally in the jaw. This procedure is an important part of oral surgery and is carried out by an Oral and Maxillofacial Surgeon to ensure safety and precision.
Why Surgical Tooth Removal Is Necessary
Certain conditions make surgical tooth removal necessary:
- Impacted teeth: Teeth trapped under the gum or bone, which cannot erupt normally.
- Broken or fractured teeth: Teeth that have fractured due to trauma or decay, making conventional extraction impossible.
- Abnormal positioning: Teeth that are tilted, rotated, or otherwise difficult to remove.
- Infection or abscess: Severe dental infections that threaten surrounding teeth or bone.
- Preparation for orthodontics: In some cases, teeth need to be removed surgically to make room for proper alignment.
Surgical removal is often preferred over attempting a forceful extraction, as it minimizes the risk of damage to nearby teeth, nerves, and bone.
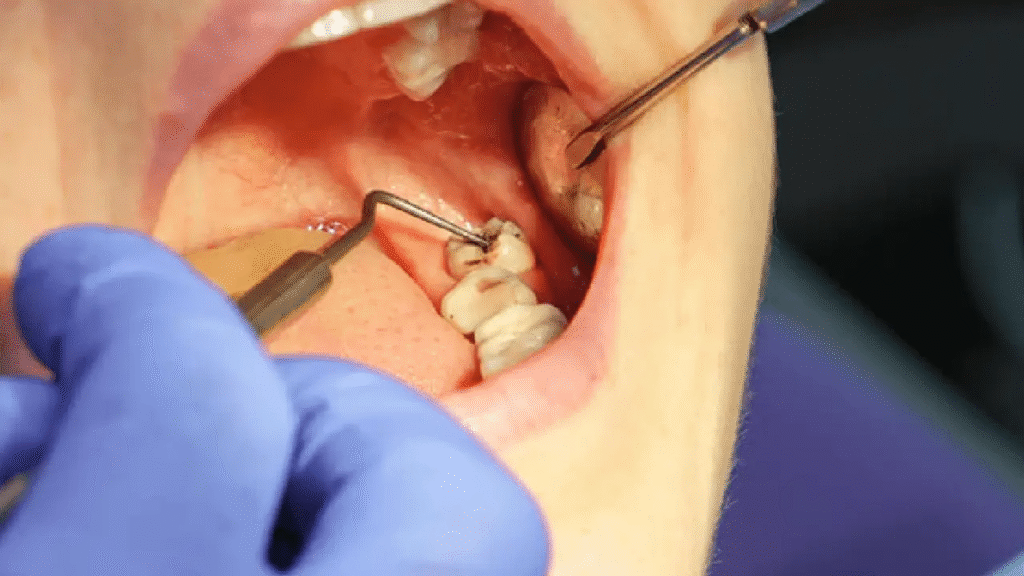
How Surgical Tooth Removal Is Performed
Before surgery, the oral surgeon evaluates the tooth using X-rays or 3D imaging to understand its position and plan the procedure. The surgical process typically involves the following steps:
- Anesthesia: Local anesthesia is applied to numb the area, and sedation or general anesthesia may be used for more complex cases.
- Incision: The surgeon makes an incision in the gum to access the tooth. For impacted teeth, part of the surrounding bone may be removed.
- Tooth Removal: Depending on the tooth’s position, it may be removed in sections. This reduces trauma and ensures a smoother extraction.
- Cleaning and Closure: The site is thoroughly cleaned, and sutures may be placed to help the gum heal. Dissolvable stitches are often used for patient convenience.
Recovery and Aftercare
Recovery after surgical tooth removal varies depending on the complexity of the procedure. Proper post-operative care ensures faster healing and reduces the risk of complications. Important aftercare steps include:
- Applying ice packs to reduce swelling in the first 24 hours.
- Eating soft foods and avoiding hard, crunchy, or sticky foods for a few days.
- Taking prescribed painkillers and antibiotics to prevent infection.
- Keeping the mouth clean using gentle rinsing with warm salt water.
- Avoiding smoking, alcohol, and straws, which can dislodge the blood clot and cause dry socket.
Benefits of Surgical Tooth Removal
- Resolves pain caused by impacted or damaged teeth.
- Prevents infections from spreading to adjacent teeth or bone.
- Corrects alignment issues and prepares the mouth for orthodontic or restorative procedures.
- Reduces the risk of cysts, tumors, or other complications associated with problematic teeth.
Surgical tooth removal is a safe and effective procedure when performed by a qualified oral surgeon. With proper care and follow-up, patients can recover comfortably and maintain long-term oral health.
Dental Implant Surgery
Dental implant surgery is a modern and highly effective procedure for replacing missing teeth. Unlike removable dentures or bridges, dental implants provide a permanent solution that looks, feels, and functions like natural teeth. This procedure involves surgically placing a small titanium post into the jawbone, which serves as an artificial tooth root. Once the implant integrates with the bone, a dental crown is attached to restore the tooth’s appearance and function. Dental implant surgery is performed by an Oral and Maxillofacial Surgeon or a qualified dental implant specialist.
Why Dental Implant Surgery Is Needed
Dental implants are recommended in several situations:
- Missing teeth: One or more teeth lost due to decay, trauma, or gum disease.
- Unstable dentures or bridges: Patients who find removable dentures uncomfortable or unstable.
- Jawbone preservation: Dental implants help maintain jawbone density and prevent bone loss after tooth loss.
- Improved oral function: Implants restore natural chewing and speaking abilities, which may be compromised with missing teeth.
- Aesthetic restoration: Implants provide a natural-looking solution, improving facial appearance and confidence.
Dental implants are often considered the gold standard for tooth replacement due to their durability, functionality, and long-term benefits.
How Dental Implant Surgery Is Performed
Before the procedure, the surgeon evaluates the patient’s oral health using X-rays or 3D scans. This ensures there is sufficient bone to support the implant and helps plan the optimal placement.
- Anesthesia: Local anesthesia, sedation, or general anesthesia is used depending on the complexity of the case and patient comfort.
- Implant Placement: The surgeon makes a small incision in the gum and drills a hole into the jawbone where the titanium implant is inserted.
- Healing and Osseointegration: The implant is left to integrate with the bone, a process called osseointegration, which usually takes a few months. This ensures stability and strength.
- Abutment and Crown Placement: Once healing is complete, an abutment is attached to the implant, and a custom-made crown is placed on top, completing the restoration.
Recovery and Aftercare
Recovery from dental implant surgery generally takes a few days to a week for initial healing, with complete osseointegration taking several months. Proper care ensures long-term success:
- Maintain oral hygiene by brushing and rinsing gently around the implant site.
- Avoid hard, sticky, or crunchy foods during the initial healing period.
- Take prescribed antibiotics and painkillers as directed.
- Attend follow-up appointments to monitor healing and implant integration.
Benefits of Dental Implants
- Restores natural tooth function for chewing and speaking.
- Provides a long-lasting and durable solution for missing teeth.
- Prevents jawbone deterioration and preserves facial structure.
- Enhances appearance and boosts confidence.
- Minimizes the risk of shifting teeth and bite problems compared to removable dentures.
Dental implant surgery is a reliable and effective solution for patients seeking permanent tooth replacement. With proper planning, expert surgical execution, and good post-operative care, dental implants can provide lifelong benefits and significantly improve oral health and quality of life.
Cyst and Tumor Removal in the Mouth
Cyst and tumor removal in the mouth is an important type of oral surgery performed to eliminate abnormal growths that develop in the jaw, gums, or soft tissues of the oral cavity. While some cysts and tumors are benign, others can pose serious health risks if left untreated. Removing these growths surgically not only preserves oral health but also prevents complications that could affect surrounding teeth, bone, and facial structures. Oral surgeons specialize in diagnosing and treating these conditions with precision and care.
Why Cyst and Tumor Removal Is Needed
Cysts and tumors in the mouth can cause several problems, including:
- Bone damage: Large cysts or tumors can erode jawbone, weakening the structure.
- Displacement of teeth: Growths may push adjacent teeth out of alignment, affecting bite and function.
- Pain and discomfort: Some cysts or tumors cause swelling, tenderness, or persistent pain.
- Infection: Certain cysts can become infected, leading to abscesses and other complications.
- Malignancy: While most cysts are benign, some tumors may be precancerous or cancerous. Early detection and removal are critical to prevent serious health risks.
Surgical removal is often the most effective solution to these problems, ensuring both treatment and diagnosis through tissue analysis.
How Cyst and Tumor Removal Is Performed
Before surgery, the oral surgeon evaluates the cyst or tumor using X-rays, CT scans, or MRI to determine size, location, and relation to surrounding structures. A biopsy may be performed to assess whether the growth is benign or malignant.
- Anesthesia: Local anesthesia, sedation, or general anesthesia is administered depending on the complexity and size of the growth.
- Incision and Access: The surgeon makes an incision in the gum or oral tissue to reach the cyst or tumor. If it is located in the jawbone, a small portion of bone may be removed to access it safely.
- Removal: The entire cyst or tumor is carefully excised. In cases of larger growths, the surgeon may remove the tissue in sections.
- Cleaning and Closure: After removal, the area is thoroughly cleaned to prevent infection, and sutures may be placed to promote healing.
- Biopsy: The removed tissue is sent to a laboratory for histopathological analysis to confirm its type and ensure no malignant cells are present.
Recovery and Aftercare
Recovery varies depending on the size and complexity of the procedure. Important steps include:
- Maintaining oral hygiene with gentle rinsing to avoid infection.
- Eating soft foods during the initial healing period.
- Taking prescribed antibiotics and pain medication as directed.
- Avoiding smoking, alcohol, or strenuous activities that may affect healing.
- Attending follow-up appointments to monitor recovery and assess for any recurrence.
Benefits of Cyst and Tumor Removal
- Prevents damage to jawbone and surrounding teeth.
- Relieves pain, swelling, and discomfort.
- Reduces the risk of infection and other complications.
- Ensures early detection and treatment of potential malignancies.
- Restores normal oral function and aesthetics.
Cyst and tumor removal in the mouth is a critical oral surgery procedure that safeguards both dental and overall health. Early diagnosis, expert surgical intervention, and proper post-operative care ensure successful treatment and long-term oral well-being.
Jaw Correction Surgery (Orthognathic Surgery)
Jaw correction surgery, also known as orthognathic surgery, is a specialized oral surgical procedure designed to correct abnormalities of the jaw and facial structure. This surgery is performed when the upper or lower jaw is misaligned, causing functional problems such as difficulty chewing, speaking, or breathing. In addition to functional improvement, jaw correction surgery can also enhance facial symmetry and overall aesthetics. The procedure is typically carried out by an Oral and Maxillofacial Surgeon in collaboration with orthodontists.
Why Jaw Correction Surgery Is Needed
Jaw misalignment can lead to several oral and facial issues:
- Bite problems (malocclusion): Overbite, underbite, crossbite, or open bite can make chewing and speaking difficult.
- Temporomandibular joint (TMJ) disorders: Misaligned jaws can cause jaw pain, clicking, or difficulty opening and closing the mouth.
- Sleep apnea and breathing problems: Severe jaw misalignment can obstruct the airway, leading to sleep-related breathing disorders.
- Facial asymmetry: Uneven jaw growth can affect appearance and self-confidence.
- Worn teeth and dental complications: Misaligned jaws can cause excessive wear, tooth damage, and gum problems over time.
When orthodontic treatments alone are insufficient to correct these issues, jaw surgery becomes necessary to reposition the jaws properly.
How Jaw Correction Surgery Is Performed
The procedure begins with thorough planning, including X-rays, 3D imaging, and dental impressions. The surgeon assesses jaw size, shape, and alignment to determine the optimal surgical approach.
- Anesthesia: The patient is given general anesthesia to ensure complete comfort during surgery.
- Surgical Procedure: The surgeon makes precise incisions inside the mouth or, in some cases, externally, depending on the jaw structure. The upper jaw (maxilla), lower jaw (mandible), or both may be repositioned.
- Fixation: Plates, screws, or wires are used to stabilize the jaws in their new position. These materials are usually titanium and are safe for long-term use.
- Closure and Recovery: Incisions are sutured, and the patient is monitored in recovery. Postoperative care and follow-ups are critical to ensure proper healing and alignment.
Recovery and Aftercare
Recovery from jaw correction surgery is gradual and may take several weeks to months for full healing. Important post-operative care steps include:
- Following a soft or liquid diet initially to reduce stress on the jaw.
- Maintaining oral hygiene to prevent infection.
- Taking prescribed medications, including pain relievers and antibiotics.
- Attending regular follow-up appointments with both the surgeon and orthodontist.
- Performing jaw exercises as recommended to restore normal function and strength.
Patients may experience swelling, bruising, and temporary numbness during the initial recovery period, but these symptoms usually improve over time.
Benefits of Jaw Correction Surgery
- Corrects bite and chewing difficulties, improving oral function.
- Reduces jaw pain and TMJ-related issues.
- Enhances facial symmetry and overall appearance.
- Improves speech and breathing in cases of severe jaw misalignment.
- Prevents long-term dental problems, including tooth wear and gum disease.
Jaw correction surgery is a highly effective solution for individuals with significant jaw misalignment or facial abnormalities. When combined with orthodontic treatment and proper post-operative care, it can significantly improve both oral health and quality of life.
Frenectomy – Lip or Tongue Tie Surgery
A frenectomy is a minor oral surgical procedure performed to correct a tight or restrictive frenulum—the small band of tissue that connects the tongue to the floor of the mouth (lingual frenulum) or the upper lip to the gum (labial frenulum). When the frenulum is too short or tight, it can restrict movement, causing functional problems with speech, eating, oral hygiene, or breastfeeding in infants. Frenectomy surgery is a simple yet effective way to improve oral function and prevent long-term complications.
Why Frenectomy Is Needed
A tight or abnormal frenulum can cause several issues:
- Tongue-tie (Ankyloglossia): Restricted tongue movement can affect speech development, make it difficult to lick, chew, or swallow, and sometimes lead to dental problems.
- Lip-tie: A restrictive upper lip frenulum can interfere with lip movement, affect dental alignment, or create gaps between front teeth (diastema).
- Infant feeding difficulties: In babies, a tight frenulum can make breastfeeding challenging, causing poor latch, slow weight gain, or nipple pain for the mother.
- Oral hygiene issues: Limited tongue or lip mobility can prevent proper cleaning of teeth and gums, increasing the risk of cavities and gum disease.
- Speech difficulties: Certain sounds may be difficult to pronounce due to restricted tongue movement.
A frenectomy addresses these problems by releasing the tight tissue and allowing normal movement of the tongue or lip.
How Frenectomy Surgery Is Performed
Frenectomy is typically a quick and minimally invasive procedure, often performed in a dental clinic. The steps include:
- Anesthesia: Local anesthesia is administered to numb the area. In infants, some procedures may be performed with topical anesthesia or minimal sedation.
- Tissue Release: The surgeon carefully cuts or removes the restrictive portion of the frenulum. In some cases, laser technology is used for a precise and bloodless procedure.
- Suturing (if needed): Depending on the technique, dissolvable sutures may be placed to aid healing. Laser frenectomy often does not require sutures.
- Immediate Evaluation: The surgeon checks the range of motion after the procedure to ensure that the tongue or lip can move freely.
The procedure is usually completed within 15–30 minutes, and most patients experience minimal discomfort.
Recovery and Aftercare
Recovery from a frenectomy is typically fast, especially with modern laser techniques. Key aftercare instructions include:
- Gentle oral hygiene to prevent infection.
- Performing recommended tongue or lip exercises to maintain full mobility.
- Soft diet for the first day or two in some cases, especially for older children or adults.
- Pain management with over-the-counter medications, if necessary.
Healing is generally complete within 1–2 weeks, and most patients experience significant improvement in function shortly after the procedure.
Benefits of Frenectomy
- Improves tongue or lip movement and overall oral function.
- Enhances breastfeeding in infants.
- Prevents dental issues such as gaps or misalignment of teeth.
- Reduces speech difficulties and aids proper pronunciation.
- Minimally invasive procedure with quick recovery.
Frenectomy is a safe and effective solution for children and adults with tongue-tie or lip-tie. Early evaluation and treatment can prevent long-term complications and improve quality of life, speech, feeding, and oral health.
Trauma and Injury Management in Oral Surgery
Trauma and injury to the mouth, teeth, and jaw are common occurrences caused by accidents, sports, falls, or physical assaults. Such injuries can range from minor chipped teeth to severe fractures of the jaw and facial bones. Oral surgery plays a critical role in managing these injuries, restoring function, preventing long-term complications, and preserving the patient’s appearance. Oral and maxillofacial surgeons are specially trained to handle complex trauma cases that involve both soft tissues and bone structures in the oral and facial regions.
Common Oral and Facial Injuries
Oral and facial trauma can take many forms:
- Fractured teeth: Teeth may break partially or completely due to impact.
- Displaced or knocked-out teeth: Traumatic forces can push teeth out of their natural position or completely dislodge them (avulsion).
- Jaw fractures: The upper (maxilla) or lower jaw (mandible) may fracture, affecting chewing, speech, and alignment.
- Soft tissue injuries: Cuts, lacerations, and bruising of the lips, gums, tongue, or cheeks are common.
- Facial bone fractures: Severe trauma can involve the cheekbones, eye sockets, or nasal bones.
Immediate and proper management is essential to restore oral function, prevent infection, and maintain facial aesthetics.
How Trauma and Injury Are Managed
The approach to managing oral and facial trauma depends on the type and severity of the injury:
- Initial Assessment: The surgeon evaluates the injury using X-rays, CT scans, or other imaging techniques to identify fractures, displacements, and associated soft tissue damage.
- Emergency Care: In cases of severe bleeding, airway obstruction, or displaced teeth, immediate intervention is necessary to stabilize the patient.
- Surgical Intervention:
- Tooth stabilization: Loose or displaced teeth may be repositioned and splinted.
- Fracture repair: Broken jaws or facial bones are aligned and fixed using plates, screws, or wires.
- Soft tissue repair: Lacerations and wounds are carefully stitched or repaired to ensure proper healing and minimize scarring.
- Post-Operative Care: Pain management, antibiotics, and dietary adjustments are prescribed. Regular follow-ups monitor healing and function.
Recovery and Rehabilitation
Recovery after oral trauma depends on the complexity of the injury. Minor injuries, such as chipped teeth or small cuts, may heal in a few days to a week. More severe injuries, such as jaw fractures or multiple dental avulsions, require several weeks of recovery and rehabilitation. Important aspects of recovery include:
- Maintaining proper oral hygiene to prevent infection.
- Following dietary recommendations, usually soft foods, during initial healing.
- Performing jaw or mouth exercises if prescribed by the surgeon to restore function.
- Attending follow-up appointments to ensure proper alignment and healing.
Benefits of Oral Surgery in Trauma Management
- Restores chewing, speaking, and swallowing functions.
- Prevents long-term complications such as malocclusion or chronic pain.
- Reduces the risk of infections and abscess formation.
- Preserves facial appearance and minimizes scarring.
- Provides a safe and structured approach to complex oral and facial injuries.
Trauma and injury management in oral surgery is essential for maintaining oral function, preventing complications, and restoring facial aesthetics. Early intervention, expert surgical care, and proper post-operative management significantly improve outcomes for patients with dental and facial injuries.
Preparation Before Oral Surgery
Proper preparation before oral surgery is crucial for ensuring a safe procedure, minimizing complications, and promoting a smooth recovery. Oral surgery may include procedures such as tooth extractions, dental implants, jaw correction, or removal of cysts and tumors. Preparing physically, mentally, and practically can significantly improve the surgical outcome and overall patient experience.
Medical Evaluation and Consultation
Before surgery, the oral surgeon conducts a comprehensive evaluation of the patient’s oral and general health. This typically involves:
- Medical history review: Patients should provide information about chronic illnesses, medications, allergies, and previous surgeries. Conditions such as diabetes, hypertension, or bleeding disorders can affect surgical planning.
- Dental examination: The surgeon evaluates the teeth, gums, and jaw to identify any potential issues that may impact the surgery.
- Imaging: X-rays, panoramic scans, or 3D CT scans may be used to assess bone structure, tooth positioning, and the complexity of the procedure.
- Lab tests: Blood tests or other diagnostic tests may be requested, especially for patients with systemic health concerns.
This thorough assessment helps the surgeon plan the surgery safely and effectively.
Pre-Surgery Instructions
Following the surgeon’s instructions before oral surgery is essential. Common recommendations may include:
- Fasting: For procedures under general anesthesia or sedation, patients are often asked to avoid eating or drinking for several hours prior to surgery.
- Medication management: Certain medications, such as blood thinners, may need to be paused under the guidance of a healthcare provider. Antibiotics may also be prescribed to prevent infection.
- Avoiding smoking and alcohol: Smoking and alcohol can interfere with healing and increase the risk of complications. Patients are usually advised to abstain for at least 24–48 hours before surgery.
- Arranging transportation: Patients undergoing sedation or general anesthesia should have a responsible adult accompany them to and from the surgery.
Mental and Emotional Preparation
Surgery can be stressful, and preparing mentally can improve the patient experience:
- Understanding the procedure, risks, and expected outcomes reduces anxiety.
- Discussing fears or concerns with the oral surgeon can provide reassurance.
- Visualization or relaxation techniques, such as deep breathing, can help calm nerves before surgery.
Home Preparation
Preparing your home for post-operative recovery makes healing more comfortable:
- Stock up on soft foods and liquids, such as soups, yogurt, and smoothies.
- Prepare ice packs or cold compresses to manage swelling after surgery.
- Create a comfortable resting area with pillows and easy access to essentials.
- Ensure oral hygiene supplies, such as a soft-bristled toothbrush and salt for rinsing, are readily available.
Benefits of Proper Preparation
- Reduces surgical and anesthesia-related risks.
- Minimizes post-operative complications such as bleeding, infection, or delayed healing.
- Ensures a smoother recovery and faster return to normal activities.
- Increases patient confidence and comfort during the procedure.
Step-by-Step Oral Surgery Procedure
Oral surgery is a carefully planned process designed to treat complex dental and jaw problems that cannot be resolved with conventional dental treatments. Whether it involves tooth extraction, dental implants, jaw correction, or cyst removal, oral surgery follows a structured approach to ensure safety, effectiveness, and proper healing. Understanding the step-by-step procedure can help patients feel more prepared and confident.
Initial Consultation and Planning
The oral surgery process begins with a thorough consultation. During this phase:
- The oral surgeon reviews the patient’s medical and dental history, including any chronic illnesses, medications, or allergies.
- A detailed oral examination is conducted to evaluate the teeth, gums, and jaw.
- Imaging studies, such as X-rays, panoramic scans, or 3D CT scans, are used to assess the structure of the jaw, tooth positioning, and surrounding tissues.
- The surgeon discusses treatment options, risks, benefits, and expected outcomes, allowing the patient to make an informed decision.
Proper planning at this stage ensures the surgery is tailored to the patient’s unique needs and minimizes potential complications.
Pre-Surgical Preparation
Before the day of surgery, patients are given specific instructions to optimize safety and recovery:
- Fasting guidelines if sedation or general anesthesia is planned.
- Medication adjustments, including pausing certain drugs like blood thinners under physician guidance.
- Arranging transportation for patients who will be sedated.
- Preparing the home environment with soft foods, ice packs, and comfortable rest areas for post-operative care.
Anesthesia Administration
On the day of surgery, the patient is prepared in the surgical room, and anesthesia is administered:
- Local anesthesia numbs the surgical site for minor procedures.
- Sedation may be used for anxious patients or more complex procedures.
- General anesthesia is reserved for extensive or complicated surgeries, ensuring the patient is completely unconscious and pain-free.
The choice of anesthesia depends on the procedure type, complexity, and patient preference.
Surgical Procedure
The main surgical steps vary depending on the type of oral surgery but generally include:
- Incision or exposure: The surgeon gains access to the surgical site, which may involve lifting the gum or removing small portions of bone.
- Treatment: This can include tooth extraction, dental implant placement, jaw repositioning, cyst or tumor removal, or soft tissue repair.
- Stabilization: In cases like jaw surgery or implants, the bones or implants are stabilized using screws, plates, or sutures.
- Cleaning and closure: The area is cleaned thoroughly, and incisions are sutured to promote healing.
Throughout the procedure, sterile techniques are strictly maintained to prevent infection.
Post-Surgical Recovery
After the surgery, the patient is monitored until the effects of anesthesia wear off. Post-operative care instructions include:
- Managing pain and swelling with medications and ice packs.
- Following a soft or liquid diet for the initial healing period.
- Maintaining gentle oral hygiene to prevent infection.
- Attending follow-up appointments to monitor healing and remove sutures if necessary.
Benefits of a Step-by-Step Approach
- Ensures patient safety and minimizes surgical risks.
- Allows for precise, targeted treatment tailored to the patient’s needs.
- Promotes faster healing and reduces the risk of complications.
- Enhances patient understanding and confidence throughout the process.
Following a structured, step-by-step procedure in oral surgery ensures the best possible outcomes, combining professional expertise, patient safety, and efficient healing.
Post-Operative Care After Oral Surgery
Proper post-operative care is crucial after oral surgery to ensure healing, reduce the risk of complications, and restore oral function as quickly as possible. Whether the procedure involved tooth extraction, dental implants, jaw correction, or cyst removal, following the oral surgeon’s instructions helps patients recover comfortably and effectively.
Immediate Care After Surgery
After surgery, patients are typically monitored for a short period until the effects of anesthesia or sedation wear off. Important steps immediately following oral surgery include:
- Rest: Patients should rest for the remainder of the day and avoid strenuous activities.
- Ice packs: Applying ice to the outside of the face reduces swelling and inflammation. Typically, 15–20 minutes on and off during the first 24 hours is recommended.
- Bleeding control: Minor bleeding or oozing is common. Patients may be advised to gently bite on gauze for 30–60 minutes to control bleeding.
Pain and Swelling Management
Pain and swelling are natural parts of the healing process. To manage them effectively:
- Take prescribed painkillers as directed by the oral surgeon. Over-the-counter medications may also be recommended for minor discomfort.
- Use cold compresses during the first 24–48 hours to minimize swelling. After this period, warm compresses may help relax muscles and improve circulation.
- Keep the head elevated while resting or sleeping to reduce swelling.
Diet and Nutrition
Maintaining proper nutrition while avoiding stress on the surgical site is essential:
- Start with soft foods such as yogurt, soups, mashed vegetables, or smoothies.
- Avoid hard, chewy, or spicy foods for the first few days, as they can irritate the surgical area or dislodge sutures.
- Stay hydrated, but avoid drinking through straws, as the suction can disrupt blood clots and lead to dry socket.
Oral Hygiene
Keeping the mouth clean is vital to prevent infection:
- Gently rinse with warm salt water starting 24 hours after surgery, typically 2–3 times a day.
- Avoid vigorous rinsing or brushing the surgical site for the first few days.
- Resume gentle brushing and flossing in other areas to maintain overall oral hygiene.
Activity and Lifestyle
- Avoid smoking and alcohol, as they can slow healing and increase the risk of infection.
- Gradually return to normal activities, but avoid strenuous exercise or heavy lifting during the initial recovery period.
- Follow all post-operative instructions provided by the oral surgeon, including medication schedules and wound care.
Recognizing Complications
While most patients heal without issues, it is important to recognize signs of potential complications:
- Excessive or prolonged bleeding.
- Severe pain not relieved by prescribed medication.
- Swelling that worsens after 48–72 hours.
- Fever, pus, or foul odor from the surgical site.
If any of these occur, patients should contact their oral surgeon immediately.
Benefits of Proper Post-Operative Care
- Promotes faster and smoother healing.
- Reduces the risk of infection, dry socket, or other complications.
- Helps restore oral function, including chewing, speaking, and swallowing.
- Improves comfort and overall patient experience during recovery.
Following proper post-operative care guidelines ensures successful recovery from oral surgery. By managing pain, maintaining hygiene, following dietary recommendations, and monitoring for complications, patients can achieve optimal healing and long-term oral health.
Benefits and Possible Risks of Oral Surgery
Oral surgery encompasses a wide range of procedures, including tooth extractions, dental implants, jaw correction, cyst and tumor removal, and frenectomy. While these procedures are generally safe and effective, it is important to understand both the benefits and possible risks to make informed decisions. Oral surgeons carefully evaluate each patient to ensure that the advantages outweigh the risks.
Benefits of Oral Surgery
- Restores Oral Function
Oral surgery can improve the ability to chew, speak, and swallow. For example, surgical removal of impacted teeth or jaw correction can restore proper bite alignment, preventing discomfort and functional limitations. - Pain Relief
Many oral conditions, such as impacted wisdom teeth, cysts, or dental trauma, cause persistent pain. Surgery alleviates this pain by addressing the underlying problem directly. - Prevents Further Complications
Timely oral surgery can prevent infections, abscess formation, tooth misalignment, and bone loss. For instance, dental implants help preserve jawbone density, while cyst removal prevents bone and tissue damage. - Improves Aesthetics and Confidence
Procedures like jaw correction or dental implants enhance facial symmetry and appearance, boosting self-esteem and overall quality of life. Patients often notice improvements in both smile aesthetics and facial profile after surgery. - Long-Term Oral Health
By addressing complex dental problems, oral surgery contributes to long-term oral health. Removing problematic teeth or growths reduces the risk of recurring infections, periodontal disease, and further tooth loss. - Facilitates Other Treatments
Some oral surgeries, such as tooth removal or bone grafting, prepare the mouth for orthodontic or restorative treatments. These procedures create a foundation for successful braces, dental implants, or prosthetics.
Possible Risks of Oral Surgery
Although oral surgery is generally safe, there are potential risks, which may vary depending on the type of procedure, complexity, and the patient’s health:
- Infection
Any surgical procedure carries a risk of infection. Surgeons prescribe antibiotics and provide post-operative care instructions to minimize this risk. - Bleeding
Mild bleeding is common after oral surgery, but excessive or prolonged bleeding may occur, especially in patients with blood disorders or those taking anticoagulant medications. - Swelling and Pain
Temporary swelling, bruising, and discomfort are expected. These usually subside within a few days with proper care and pain management. - Nerve Injury
In rare cases, oral surgery may cause temporary or permanent nerve damage, leading to numbness or tingling in the lips, tongue, or chin. Surgeons take precautions to minimize this risk. - Complications from Anesthesia
Local anesthesia, sedation, or general anesthesia can have side effects, including allergic reactions, nausea, or dizziness. Anesthesia is administered by trained professionals to ensure safety. - Delayed Healing or Dry Socket
After tooth extractions, especially wisdom teeth removal, a dry socket can occur if the blood clot is dislodged. Following post-operative care instructions reduces this risk.
Balancing Benefits and Risks
While oral surgery carries certain risks, the benefits often outweigh them, especially when performed by a qualified oral surgeon. Careful planning, proper surgical technique, and adherence to post-operative instructions significantly reduce complications. Patients who undergo oral surgery can experience improved oral function, pain relief, better aesthetics, and enhanced overall health.
Oral surgery is a vital solution for managing complex dental and jaw conditions. By understanding both its advantages and potential risks, patients can make informed decisions and achieve optimal outcomes.
Oral Surgery Services and Cost in Bangladesh
Oral surgery encompasses a range of procedures aimed at treating complex dental and facial conditions. In Bangladesh, these services are offered by numerous specialized clinics and hospitals, primarily in Dhaka. Below is an overview of common oral surgery procedures and their associated costs.
Common Oral Surgery Procedures and Costs
| Procedure | Estimated Cost (BDT) | Description |
|---|---|---|
| Simple Tooth Extraction | BDT 1,000 – 2,000 | Removal of a tooth that is visible and accessible. |
| Surgical Tooth Extraction | BDT 3,000 – 5,000 | Removal of a tooth that is impacted or requires surgical intervention. |
| Wisdom Tooth Extraction | BDT 5,000 – 10,000 | Surgical removal of one or more wisdom teeth. |
| Dental Implant | BDT 50,000 – 90,000 | Placement of a titanium post to replace a missing tooth. |
| Jaw Surgery (Orthognathic) | BDT 100,000 – 200,000 | Surgical correction of jaw abnormalities. |
| Cyst or Tumor Removal | BDT 1,000 – 5,000 | Surgical removal of cysts or tumors in the oral and maxillofacial region. |
| Frenectomy (Lip or Tongue Tie Surgery) | BDT 3,000 – 5,000 | Surgical removal or modification of the frenulum to correct lip or tongue tie. |
Factors Influencing Oral Surgery Costs
- Procedure Complexity: More intricate surgeries, such as jaw corrections or tumor removals, typically incur higher costs.
- Anesthesia Type: General anesthesia may increase the overall cost compared to local anesthesia.
- Surgeon’s Expertise: Highly experienced or internationally trained surgeons may charge premium fees.
- Clinic Location and Facilities: Clinics in metropolitan areas with advanced facilities may have higher service charges.
Insurance and Payment Options
Many dental clinics in Bangladesh offer installment payment plans to ease the financial burden of oral surgeries. It’s advisable to inquire about insurance coverage, as some procedures may be partially covered under health insurance policies.
